
The People's Pharmacy
Joe and Terry Graedon
Empowering you to make wise decisions about your own health, by providing you with essential health information about both medical and alternative treatment options.
- 1 hour 5 minutesShow 1424: Breathing Better Despite Pollution, Infections, Asthma or COPD
This week, we talk with a pulmonologist–a doctor who takes care of people with lung problems. Our topics range from common respiratory infections to the hazards of breathing smoke from forest fires. We also discuss asthma and COPD. Listen to find out how you could be breathing better.
You could listen through your local public radio station or get the live stream at 7 am EDT on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on March 31, 2025.
Breathing Better Despite Infections:
We are finally emerging from an especially severe flu season. After a few years during and right after the pandemic in which there was relatively little influenza, this year was challenging. Preliminary data from the CDC suggest that between 40 million and 75 million Americans suffered from influenza or flu-like illnesses between October and March. As many as 1.2 million had to be hospitalized. The influenza viruses (there are many) are not the only pathogens that can cause coughing, fever or trouble breathing. Many others might also result in upper respiratory infections that can progress to bronchitis or lower respiratory infections and lead to wheezing or shortness of breath. A bad cold will do that for some people. Human metapneumovirus is not widely recognized and is difficult to pronounce. The infection with this virus starts like a bad cold but it produces a terrible cough that can last for weeks.
How can doctors help a patient with a respiratory infection? If the problem is influenza, they could prescribe a medicine such as oseltamivir (Tamiflu) or baloxavir (Xofluza). These medicines can shorten the duration of flu symptoms and possibly make them less severe. However, they work best when taken as soon as possible (within 48 hours) of the first symptoms appearing.
To learn whether that sore throat and sniffle is leading to flu, you might want to keep a test handy at home. There are several on the market that can determine if you have COVID-19 or influenza A. Then, if you have access to a patient portal, use it to communicate the results to your healthcare provider and get a prompt prescription.
What About a Cold?
While flu or COVID can be serious, colds are far more common. Doctors do not have much in their tool kits to help you recover from a cold, but there are a few things you can do for yourself. Spending some time in sunlight can be very useful. Dr. Seheult suspects that the benefits go beyond the amount of vitamin D you might make through that exposure. In addition, we have seen studies supporting the use of vitamin C supplements to recover from a cold more quickly.
Breathing Better with Improved Ventilation:
During the pandemic, air quality and ventilation got more attention than ever before. Now, although we may be less concerned about airborne pathogens, we still need to pay attention to air quality. Forest fires, whether in California, the Carolinas or any other part of the continent, can put out a lot of smoke. Wildfire smoke carries small particles that can penetrate deep in the lungs and do a lot of damage. Air conditioning may help clean indoor air. So can an inexpensive do-it-yourself air filtering system called a Corsi-Rosenthal box. Here is a link to the show in which we describe how to make one at home.
Struggling to Exhale:
Dr. Seheult also describes the Global Initiative for Asthma, or GINA. Asthma is reversible airway inflammation. Sometimes this is caused by allergic reactions. Infections may also cause inflammation and lead to asthma exacerbations. In the presence of inflammation, the smooth muscle around the little airways deep in the lungs constrict. This makes it difficult to exhale and make room for the next fresh new breath.
The problem is similar in chronic obstructive pulmonary disease (COPD), in that inflammation tightens those critical small airways and interferes with exhalation. That in turn can keep the patient from being able to take a good breath in. In COPD, however, the inflammation is irreversible.
Both asthma and COPD may respond to drugs that activate beta receptors (“beta agonists”). The long-acting beta agonists (LABAs) are especially prominent. Inhaled steroids can calm the inflammation in both conditions so people can start breathing better. In some instances, an antibiotic like azithromycin can reduce exacerbations. We don’t know whether it is working by fighting off hidden pathogens, or whether it is also reducing inflammation. In COPD, anticholinergic drugs may be able to relax airways even beyond the effects of the beta agonists. If calming inflammation is not good enough, people may need a rescue inhaler.
When Should You Get Emergency Attention?
People experiencing shortness of breath, especially if they are also having fevers, chills or night sweats, should get medical attention promptly.
This Week’s Guest:
Dr. Roger Seheult is an Associate Clinical Professor at the University of California, Riverside School of Medicine, and an Assistant Clinical Professor at the School of Medicine and Allied Health at Loma Linda University.
Dr. Seheult is quadruple board-certified in Internal Medicine, Pulmonary Diseases, Critical Care Medicine, and Sleep Medicine through the American Board of Internal Medicine. HIs current practice is in Beaumont, California where he is a critical care physician, pulmonologist, and sleep physician at Optum California.
He lectures routinely across the country at conferences and for medical, PA, and RT societies, is the director of a sleep lab, and is the Medical Director for the Crafton Hills College Respiratory Care Program.

Roger Seheult, MD, MedCram, Loma Linda, UC-Riverside
MedCram
In 2012 he and Kyle Allred founded MedCram L.L.C., a medical education company with CME-accredited videos that are utilized by hospitals, medical schools, and hundreds of thousands of medical professionals from all over the world (and over 1 million YouTube Subscribers). His passion is “demystifying” medical concepts and offering people the tools for staying healthy.
We have found Dr. Seheult’s MedCram videos amazing. He makes many complex medical topics understandable. This is a skill that few of Joe’s professors in the University of Michigan’s Department of Pharmacology could claim.
Dr. Seheult was the recipient of the 2021 San Bernardino County Medical Society’s William L. Cover MD Award for Outstanding Contribution to Medicine and the 2022 UnitedHealth Group’s The Sages of Clinical Service Award. In 2022 both Roger Seheult and Kyle Allred received the HRH Prince Salmon bin Hamad Al Khalifa Medical Merit Medal from the Kingdom of Bahrain for their contribution to health policy in the Kingdom of Bahrain.
Listen to the Podcast:
The podcast of this program will be available Monday, March 31, 2025, after broadcast on March 29. You can stream the show from this site and download the podcast for free. In addition to what you hear on the broadcast, the podcast also contains information about TRP channels and home remedies for coughs. We also discuss the heart drug amiodarone and its effects on the lung, along with the nature of interstitial lung disease and how to treat it. You’ll also learn about the pros and cons of OTC inhalers. Can they get you breathing better?
27 March 2025, 6:33 pm - 57 minutes 57 secondsShow 1423: How to Fix Your Foot Pain
This week, Dr. Jane Andersen joins Joe and Terry in the studio to answer listeners’ questions about foot problems. Do you have bunions or plantar fasciitis? Dr. Andersen has tips on how to fix your foot pain. We invite you to call and tell us about it. You can call 888-472-3366 between 7 and 8 am EDT. Or email us: radio@PeoplesPharmacy.com.
You could listen through your local public radio station or get the live stream at 7 am EST on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on March 24, 2025.
How Can You Fix Your Foot Pain?
If your feet don’t feel good, you won’t either. Just imagine stubbing your toe. Ouch, that hurt! But stubbed toes generally recover fairly quickly. Some other common foot problems are likely to cause more long-lasting pain. Some of these may result from participation in sports, such as sprained ankles or stress fractures. What is the best way to handle these injuries so they won’t cause persistent problems?
Preventing Foot Pain:
Are your feet flat? Find out what exercises may help and which shoes you should choose to fix your foot pain from flat feet.
Heel pain is another common problem. Inflammation of the Achilles tendon is one possible cause. Perhaps more often, plantar fasciitis triggers heel pain. That is an inflammation of the tissue connecting the heel and the ball of the foot, and special stretches can often help.
If you have wondered about heel spurs or neuromas, tell us what you would like to know. Restoring feet to good health can cover a lot of different areas.
Toes and Toenails:
How about toes? Find out what to do about hammertoes, mallet toes or claw toes, as well as bunions. Are you worried about gout? It may affect the toes first, before causing pain in other parts of the body.
With warmer weather on the way, you may be interested in learning how to prevent athletes foot or eliminate toenail fungus. Do you have corns or calluses on your feet? What is the difference between them, and do the treatments differ?
The questions listeners ask drive the topics we discuss in this show. You can email questions ahead of time to: radio@peoplespharmacy.com.
This Week’s Guest:
Dr. Jane Andersen, Board Certified, American Board of Foot and Ankle Surgery, is in practice at Chapel Hill Foot and Ankle, part of FASMA, Foot and Ankle specialists of the Mid Atlantic, in Chapel Hill, North Carolina. Dr. Andersen specializes in Foot and ankle care for Children, Adults, Athletes and Geriatric Patients including surgery and conservative care. She is a Trustee of the American Podiatric Medical Association. January 18, 2025, Jane Andersen, DPM, was awarded the Edwin B. Martin, Jr., Award for Podiatrist of the Year.

Dr. Jane Andersen can help you manage your foot problems.
Listen to the Podcast:
The podcast of this program will be available Monday, March 24, 2025, after broadcast on March 22. You can stream the show from this site and download the podcast for free.
20 March 2025, 4:31 pm - Show 1422: Can You Regain Your Sense of Smell After Illness?
This week, our guests take two different approaches to the sense of smell. We talk with a surgeon who treats people having difficulties with that sense. In addition, a nurse describes utilizing the sense of smell for aromatherapy in integrative healing. Learn about the fascinating science of smell.
You could listen through your local public radio station or get the live stream at 7 am EDT on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on March 17, 2025.
The Science of Smell:
Of all our senses, the sense of smell often gets short shrift. Aside from Marcel Proust’s evocative description of the link between odor and memory, we don’t think much about smell. Scientists have discovered, however, that much of our social interaction relies on olfaction at a subconscious level. It plays a largely unconscious role in our choice of mates as well as in the timing of sexual activity. It is also important for the bonding between mothers and their infants. Consequently, the sense of smell is crucial for the survival of our species, even when we aren’t paying attention.
Losing our sense of smell can be devastating, as too many people learned by experience during the COVID-19 pandemic. Not only did they miss out on pleasant aromas like fresh-brewed coffee or newly mown grass, but they also were at a disadvantage in detecting if there might be gas leaking in the kitchen or a fire smoldering somewhere in the house.
Although some of those who lost their sense of smell during an acute infection subsequently regained it, others did not. Too many people are still suffering from anosmia. Is there anything that can be done to help them?
Regenerating Nerves in the Nose:
Many viruses can cause inflammation in nasal tissue and potentially damage the sense of smell. During COVID-19, the SARS-CoV-2 virus attacked ACE receptors on cells in the olfactory epithelium of the nose. These cells are not the nerve cells themselves, but support cells (called, if you must know, sustentacular cells). Fortunately, these cells can regenerate, although it takes time.
The Science of Smell Recovery–Olfactory Training:
The first step in recovering the sense of smell is olfactory training. It could be considered something like physical therapy for the nose. In this structured smelling protocol, people are exposed to one of four distinctive aromas from essential oils: lemon, rose, eucalyptus or clove. As they attempt to discern the scent, they remember how they used to experience those odors. As part of the protocol, they also irrigate their nasal passages with high-dose steroids in saline solution (International Forum of Allergy & Rhinology, Sep. 2018). Over many months, this concerted effort is able to help 30 to 50 percent of patients recover their sense of smell to a satisfactory degree.
The Science of Smell Recovery–Platelet-Rich Plasma:
To help people who are not successful enough with olfactory training, Dr. Zara Patel has pioneered the use of platelet-rich plasma. PRP injections have been used to help athletes recover from injury. Since it can be helpful in situations where inflammation is high, she tried PRP injections for people with difficulty smelling. A randomized controlled trial showed that the injection is safe and may be effective in helping people recover their sense of smell after COVID-19 (International Forum of Allergy & Rhinology, June 2023). She hopes to conduct a larger study that would be more conclusive.
Harnessing the Sense of Smell with Aromatherapy:
Dr. Patel was careful to point out the distinction between olfactory training, based on the science of smell, and aromatherapy. Our other guest, an integrative care nurse, utilizes aromatherapy to help people in post-anesthesia care units. There is some evidence, for example, that the aroma of lavender essential oil can help anxious patients relax and get to sleep, but better studies are necessary (Phytomedicine, Dec. 2019).
Plants use the volatile compounds in their essential oils for communication. In addition, some terpenes in juniper or pine have antiviral activity, while components in clary sage or bergamot have antifungal properties. Nurses in some cancer hospitals utilize aromatherapy to help patients overcome nausea and pain associated with chemotherapy. This is an area of the science of smell in which our guest Kathy Fritze has special expertise.
This Week’s Guests:
Zara M. Patel, MD, is Professor of Otolaryngology-Head and Neck Surgery at the Stanford School of Medicine. Her website is https://profiles.stanford.edu/zara-patel

Zara Patel, MD, Stanford School of Medicine
Kathy Fritze, RN, BSN, is a holistic and integrative care nurse in the Wellness & Support Center at the University of Maryland St. Joseph Medical Center.

Kathryn Fritze RN, BSN
Listen to the Podcast:
The podcast of this program will be available Monday, March 17, 2025, after broadcast on March 15. You can stream the show from this site and download the podcast for free. In addition to what you heard in the broadcast, the podcast includes additional information on why people sometimes detect strange odors that others don’t perceive. We also discuss people who have strong reactions to odors in perfume or detergent, such that they become physically ill when they smell them.
14 March 2025, 1:37 am - 1 hour 6 minutesShow 1421: Is Lp(a) the Heart Risk No One Talks About?
This week, we get in-depth information on Lp(a), the heart risk no one talks about. You have heard of cholesterol, and you may even know what your cholesterol level is. The compound lipoprotein a may be equally dangerous when it is elevated, but you have probably heard very little about it.
You could listen through your local public radio station or get the live stream at 7 am EDT on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on March 10, 2025.
What Is Lp(a)?
Lipoprotein a, or L-P-little a for short, circulates in the bloodstream, where it picks up and carries cholesterol and oxidized phospholipids. Scientists believe that blood levels are determined mostly by genetics and change very little over the course of our lives. Roughly 20 percent of people have high levels of Lp(a), above 30 ng/dL or 75 nmol/L. The two different figures are because tests use different units to measure the blood concentration, either nanograms per deciliter or nanomols per liter.
While we don’t know if Lp(a) has or perhaps once had some important functions, we do know that elevated levels of this chemical is associated with heart disease. People with higher levels are more likely to suffer blood clots and inflammation. That puts them at risk for heart attacks or even strokes. So why hasn’t your doctor ordered a blood test to learn your level?
Is Lp(a) the Heart Risk Doctors Can’t Treat?
Perhaps doctors have been reluctant to measure or discuss lipoprotein a because they don’t have good interventions. That is beginning to change with the development of antisense oligonucleotides, a new category of prescription drugs that can cut levels sharply. The FDA has not yet approved any of these new medications, though. The first of these, pelacarsen, is still in Phase 3 trials needed before the agency can consider the evidence. However, it can bring down lipoprotein a by an estimated 80 percent.
Cardiologists’ favorite drugs, statins, do not help Lp(a) levels. In fact, Lp(a) the heart risk rises when people are taking statins to lower their cholesterol. Other cholesterol-lowering drugs such as evolocumab (Repatha) and alirocumab (Praluent) can bring Lp(a) levels down modestly. One really old cholesterol-lowering drug, high-dose niacin, also helps moderate Lp(a). Some people do not tolerate it, however, as it can cause very uncomfortable flushing. So far as we know, no scientists have run studies to see whether niacin reduces the risk of heart attacks and other complications because of its effects on Lp(a).
Other Complications of Lp(a):
Our guest, Dr. Sam Tsimikas, is among the country’s leading experts on lipoprotein a. We asked him whether Lp(a) the heart risk factor causes other problems as well. Dr. Tsimikas described heart failure, potentially resulting from a heart attack, as well as peripheral artery disease (PAD), which can make it painful to walk. Lp(a) seems to cause plaque in arteries throughout the body. As a result, it can increase the chance of a stroke. In addition, it contributes to calcification of the heart valves. This condition interferes with their ability to function properly.
What Can We Do If Lp(a) Is Too High?
Dr. Tsimikas runs a unique clinic for cardiology patients with high levels of Lp(a). We asked him how he helps them. One approach is to collect additional information about their level of risk. A coronary calcium score can be a useful indicator. If it is high, he and his patients work to control all the potential risk factors that they can. He discusses the potential benefit of aspirin with them. Because Lp(a) the heart risk factor increases the chance of dangerous blood clots, the anti-clotting activity of aspirin can sometimes be helpful.
Offering dietary advice can be tricky if a patient has high cholesterol as well as elevated Lp(a), since the ideal diets for each are nearly opposite each other. A ketogenic diet tends to raise LDL cholesterol, for example, while it may modestly lower Lp(a). We think by the end of this episode, you’ll join us in hoping that scientists can learn a lot more about Lp(a) in the next few years.
This Week’s Guest:
Sotirios (Sam) Tsimikas, MD, FACC, FAHA, FSCAI, is Professor of Medicine/Cardiology and Director of Vascular Medicine at the Sulpizio Cardiovascular Center. That is part of the Division of Cardiovascular Medicine at the University of California, San Diego. His website is https://profiles.ucsd.edu/sotirios.tsimikas

Sotirios (Sam) Tsimikas, MD, FACC, FAHA, FSCAI, UCSD
Listen to the Podcast:
The podcast of this program will be available Monday, March 10, 2025, after broadcast on March 8. You can stream the show from this site and download the podcast for free. In addition to what you heard in the broadcast, the podcast includes additional information on calcium scores and the benefits and risks of statins to lower cholesterol.
7 March 2025, 2:28 am - 1 hour 17 minutesShow 1420: The Cooking Oil Controversy Spotlights Cancer
This week, we dig into the cooking oil controversy. For decades, we’ve heard that we should be using vegetable oils rather than butter, lard or other fats (possibly even olive oil). Oils from corn, soybeans, sunflower or safflower seeds are rich in polyunsaturated fatty acids. Consequently, people consuming them may have lower cholesterol levels than those primarily using saturated fats. But could there be a downside? We hear from scientists who have found these seed oils may be linked to certain cancers.
You could listen through your local public radio station or get the live stream at 7 am EDT on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on March 3, 2025.
The Cooking Oil Controversy:
The more we learn about fats, the more it seems that focusing on just one aspect may be too simplistic. In the 1990s, health experts told Americans to avoid all fat. When it became clear that low-fat diets were not necessarily making everyone healthy, we got the message that we needed to stick with polyunsaturated fatty acids (PUFAs) like those in corn or canola oil. There are, however, different types of PUFA. Chemists classify them as omega-3, omega-6 and omega-9 fatty acids. Only omega-3 and omega-6 are considered essential fatty acids.
Current cooking oils have a preponderance of omega-6 fatty acids. As a result, the ratio of omega-6 to omega-3 in our blood has risen from a pre-industrial average of an estimated 4:1 to our current ratios of 20:1 (Missouri Medicine, Sep-Oct. 2021). This could have biological consequences.
Dietary Fat and Cancer:
Dr. William Aronson has asked how different types of dietary fat affect the progression of prostate cancer. Laboratory studies show that a diet high in corn oil accelerates the growth of human prostate cancer tumors implanted under the skin of mice. That inspired him and his colleagues to conduct a randomized controlled trial (Journal of Clinical Oncology, Dec. 13, 2024).
Fish Oil vs. Prostate Cancer:
For their trial, they recruited 100 men diagnosed with prostate cancer who opted for active surveillance rather than immediate surgery or radiation. They assigned these volunteers to different diets for one year. One group followed their usual diet and did not take fish oil. The researchers instructed the other group in avoiding omega-6 fats in their diet, increasing the amount of omega-3 rich fish and taking fish oil supplements. Minimizing omega-6 fats meant staying away from fried foods, cooking oils, bottled salad dressing and mayonnaise. At the end of the year, there was a significant difference in an important prostate cancer biomarker called Ki-67.
Does the Cooking Oil Controversy Extend to Other Cancers?
We spoke with Dr. Timothy Yeatman about his research on colorectal tumors. His research was published in Gut, a leading journal for gastroenterologists (Dec. 20, 2024). He and his colleagues used a technique called lipidomics for their analysis. They found that the lipid profile of the tumors and their micro-environments is pro-inflammatory. They seem to lack the resolving mediators (“resolvins”) that should normally accompany healing. The balance has been disrupted.
Dr. Yeatman suspects that some of this disruption may be due to changes in the microbiome that constitutes a lot of the immediate environment for colorectal tumors. He suggests that extensive use of seed oils high in pro-inflammatory omega-6 fatty acids may contribute to the imbalance. You can find soybean oil, for example, in many foods where you might not expect it, such as breads, cakes, cookies, crackers, chips and even hummus. Cooking at home allows people to avoid seed oils, but it takes time, skills and resources that are not available to everyone.
Can We Resolve the Cooking Oil Controversy?
Neither of the studies we discuss during this episode is definitive. Scientists need more research to be able to make solidly evidence-based recommendations. However, both our guests would suggest we need not wait for the final word to reduce the inflammatory potential of our diets. Reading labels carefully is a good first step to avoiding some of the seed oils that provide excess omega-6 fats and gravitate more toward omega-3 fats.
This Week’s Guests:
William Aronson, MD, is Professor in the Department of Urology of the David Geffen School of Medicine at the University of California, Los Angeles. He is also Chief of Urologic Oncology at the West Los Angeles Veterans Affairs Medical Center and Chief of Urology at the Olive View-UCLA Medical Center.
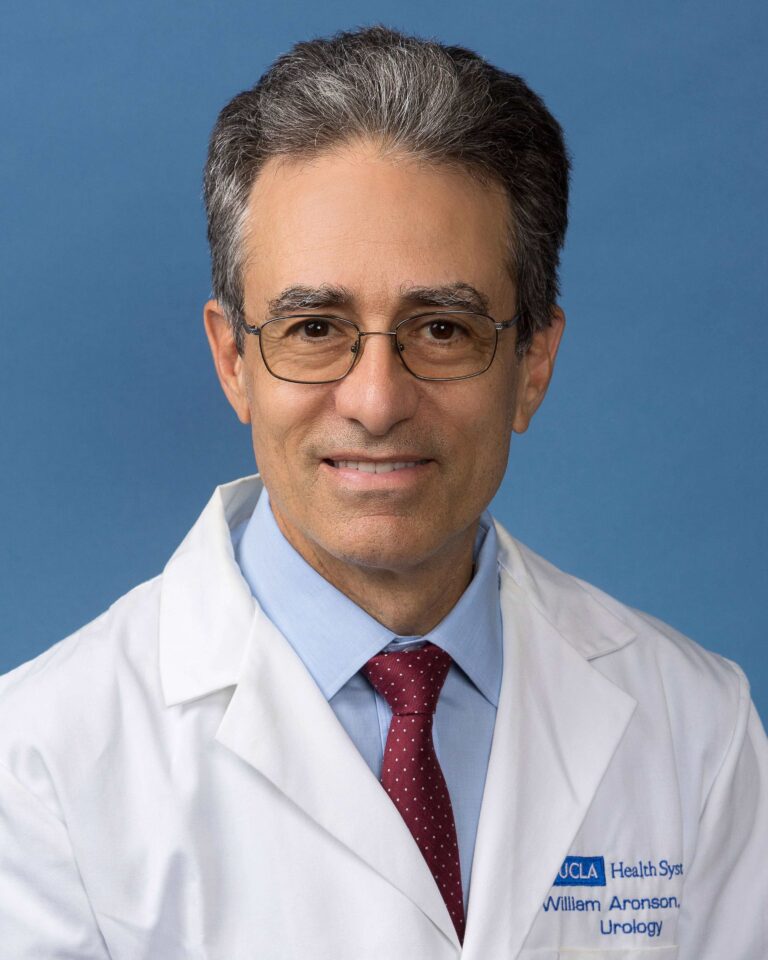
Dr. William Aronson, UCLA
Timothy Yeatman, MD, FACS, is Professor in the Dept of Surgery at the University of South Florida. He is also Associate Center Director for Translational Science and Innovation Tampa General Hospital Cancer Institute. His website is https://phenomehealth.org/c-suite/tim-yeatman-md-facs

Timothy Yeatman, MD, University of South Florida
Debora Melo vanLent, PhD, is Assistant Professor at the Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases at UT Health in San Antonio, TX. Her interview is part of the podcast.
Listen to the Podcast:
The podcast of this program will be available Monday, March 3, 2025, after broadcast on March 1. You can stream the show from this site and download the podcast for free. In addition to what you heard in the broadcast, the podcast also includes our discussion with Dr. Melo vanLent on her research into the link between dietary inflammation and dementia.
26 February 2025, 4:39 pm - 58 minutes 57 secondsShow 1419: Restless Legs, Muscle Cramps and Sleepless Nights
This week, Terry and Joe welcome Dr. Andrew Spector to the studio to share his expertise with listeners. Restless legs syndrome (RLS) is a relatively common problem that can really wreak havoc on a good night’s sleep. Have you experienced this problem? How do you manage it? We invite you to call and tell us about it. You can call 888-472-3366 between 7 and 8 am EST. Or email us: radio@PeoplesPharmacy.com.
You could listen through your local public radio station or get the live stream at 7 am EST on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on February 24, 2025.
What Is Restless Legs Syndrome?
This neurological condition is not new. The first description appeared late in the 17th century. However, it wasn’t until fairly recently that doctors started studying this problem so they could offer effective treatments. Usually RLS starts with an uncomfortable feeling in the legs that is relieved only by moving them. Sometimes people report a sensation similar to ants crawling on them. Others describe legs that throb or itch. Occasionally, the sensation will affect another body part, though legs pose the most common problem by far. The symptoms are noticeable when a person is resting, especially at the end of the day. However, sitting still for a long plane ride can also be very uncomfortable.
Do You Have Restless Legs Syndrome?
Dr. Spector will describe how he diagnoses RLS as well as other conditions that may sometimes make a diagnosis more confusing. Restless legs are not usually painful, so pain that keeps a person awake might be due to neuropathy. Another condition that often bothers a bed partner more than the patient is periodic limb movements of sleep. The name is descriptive, and because the person doesn’t wake up and isn’t troubled by unpleasant sensations, it is different from restless legs.
What Can You Do About RLS?
According to Dr. Spector, research points to low iron in the brain as a common contributor to RLS. Consequently, iron supplements could often be helpful. He’ll describe the testing that a doctor would use to determine the appropriate protocol for boosting iron.
Medications That Make RLS Worse:
If you have RLS, you may have considered taking an over-the-counter sleep aid containing diphenhydramine. Many listeners have told us that these medicines seem to make the RLS symptoms worse.
Can You Manage RLS Without Drugs?
We have heard from many people who have developed non-drug approaches that help them overcome their restless legs. They may avoid sugar or caffeine, which can sometimes trigger a bout of RLS. Avoiding nicotine and alcohol may also be useful. Magnesium or selenium supplements help certain individuals. Some listeners put a bar of soap under the bottom sheet near their legs and find that their symptoms are less troublesome. This home remedy is even more popular as a way to ward off nocturnal leg cramps. We have also heard from sufferers who have sought out acupuncture and found it effective. Maintaining a moderate level of exercise benefits many people with RLS.
Treating RLS:
In the past few decades, the FDA has approved several prescription drugs that can ease the symptoms of restless legs syndrome. It started with ropinirole (Requip), a drug that was originally developed to treat Parkinson disease. It is effective for RLS, although it has side effects that may limit its usefulness for some people. Other drugs in the same category are pramipexole (Mirapex) and rotigotine (Neupro).
If a patient cannot tolerate one of these medicines, or if the doctor decides they are not appropriate, there are other options. Doctors may prescribe a medicine such as gabapentin enacarbil (Horizant). Other drugs in this category include gabapentin or pregabalin. Although the FDA has not approved them specifically for RLS, doctors sometimes find them helpful. They frequently cost less than Horizant. Opioids and benzodiazepines offer additional prescription options. If you have experience with any of these medicines, we’d love to hear about it.
This Week’s Guest:
Andrew Spector, MD,is an Associate Professor in the Department of Neurology at the Duke University School of Medicine. Along with his clinical practice in sleep medicine, he serves as the Program Director of the Sleep Medicine Fellowship, the Duke Athletics Sleep Optimization Consultant, and the Vice Chair for Professionalism, Inclusion, Diversity, and Empowerment. Dr. Spector is the author of Navigating Life with Restless Legs Syndrome. His website is http://www.andrewspectormd.com

Andrew Spector, MD, Duke University Department of Neurology
The People’s Pharmacy is reader supported. When you buy through links in this post, we may earn a small affiliate commission (at no cost to you).
Listen to the Podcast:
The podcast of this program will be available Monday, February 24, 2025, after broadcast on Feb. 22. You can stream the show from this site and download the podcast for free.
20 February 2025, 12:19 am - Show 1418: More About the Pros and Cons of Water Fluoridation (Part 2)
This week, we offer the second of a two-part series on the pros and cons of water fluoridation. Last week we discussed the practice of adding fluoride to drinking water to prevent tooth decay. This week we hear from a researcher who has found that early exposure to fluoridated water may affect youngsters’ IQ.
You could listen through your local public radio station or get the live stream at 7 am EDT (February 15, 2025) on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on February 17, 2025.
More About the Pros and Cons of Water Fluoridation:
Some people are opposed to any municipality putting fluoride in its water supply simply because it means the residents have little choice but to use it. On the other hand, many people embrace a “no harm, no foul” philosophy. What are the potential cons of water fluoridation?
Is Fluoride a Neurotoxin?
Dr. Bruce Lanphear studied the effects of lead on children’s developing brains for decades. There is no longer any doubt that lead harms their intellectual capacity. When someone asked him about fluoride, he realized that he did not know what the potential impact on infants might be. He took advantage of an opportunity to study it, and what he and his colleagues found is rather alarming (JAMA Pediatrics, Aug. 19, 2019).
There were 512 pairs of mothers with their babies in the study, which evaluated fluoride in drinking water and also tested the mothers’ urine during pregnancy. As the levels of fluoride rose, the IQ scores of the boys, tested between age three and four, dropped. Girls did not demonstrate such an association.
The Cons of Water Fluoridation:
We encounter fluoride in toothpaste, in medications and in food packaging, among other sources. However, water fluoridation is far and away the main source of fluoride. As a result, if a community decided that the cons of water fluoridation outweigh the benefits, it would be relatively easy to lower levels for everyone. Simply stop adding fluoride to the water!
Interactions That Could Cause Trouble:
Iodine:
Another disquieting discovery from Dr. Lanphear’s research is that there are multiple interactions among the various compounds we encounter every day. For example, little boys whose mothers were able to get access to adequate iodine during pregnancy were much less likely to suffer IQ deficits than those whose mothers did not have adequate iodine (Science of the Total Environment, April 15, 2023). Hypothyroidism may be an important link.
Lead:
Another interaction is with lead. Not only does lead itself harm children’s brains, it appears to be a risk factor for tooth decay. Would that lead parents to increase the fluoride exposure for their youngsters? How do lead and fluoride interact in the body? We don’t yet have answers for these important questions.
Pesticides:
In addition, women exposed to higher levels of pesticides are more likely to give birth to children with autism if their folate levels are subpar. That is another area where researchers are striving to learn more about interactions that put babies at risk.
During the interview, we mentioned a recent meta-analysis of 74 studies of water fluoridation. You can find it in JAMA Pediatrics (Jan. 6, 2025). As with the study Dr. Lanphear describes, children exposed to higher levels of fluoride as measured in their pregnant mothers’ urine were more likely to have deficits in IQ.
The Precautionary Principle:
We asked Dr. Lanphear about the precautionary principle applied by European regulators. He suggested that it is easier to understand when stated as the medical precept, “First, do no harm!” The idea is that we should know as much as possible about hazards as well as benefits of new compounds before broad populations are exposed to them.
This Week’s Guests:
Gary D Slade, BDS, DDPH, PhD, is the John W. Stamm Distinguished Professor of Dentistry at the University of North Carolina Adams School of Dentistry in Chapel Hill, NC. He conducts epidemiological studies of oral diseases including public health interventions for prevention of dental decay. His website is https://dentistry.unc.edu/people/gary-slade/ Dr. Slade was the featured guest in last week’s episode emphasizing the benefits of water fluoridation.

Gary Slade, BDS, DDPH, PhD, is the John W. Stamm Distinguished Professor of Dentistry at the University of North Carolina Adams School of Dentistry in Chapel Hill, NC.
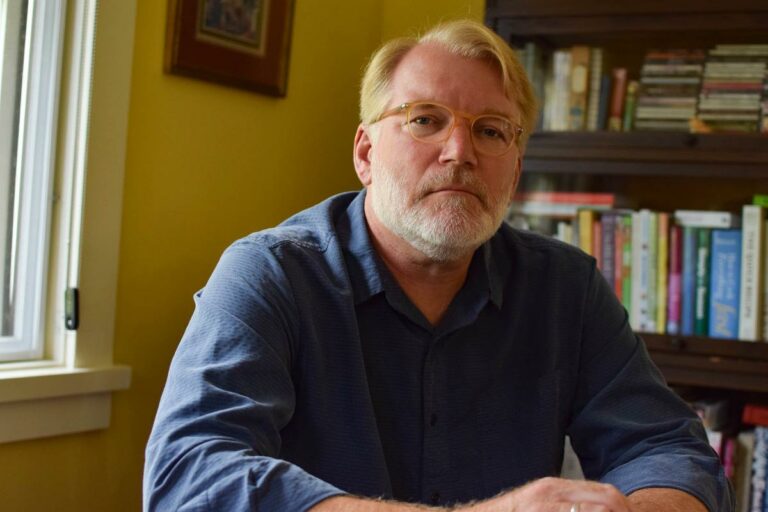
Bruce Lanphear, MD, MPH, is Professor of Health Sciences at Simon Fraser University in Burnaby, BC. He is the featured guest this week on our episode examining the cons of water fluoridation. His website is https://www.sfu.ca/fhs/about/people/profiles/bruce-lanphear.html
Professor Lanphear’s research, at the intersection of preventive medicine, pediatrics, public health, toxicology, and infectious disease, is driven by a commitment to prevent death, disease, and disability. He has published over 350 peer-reviewed studies about the impact of toxic chemicals on intellectual deficits, behavioral problems, and brain structure in children. He is ranked among the top 1% of most-cited scientists globally. Bruce and his brother, Bob, co-founded Little Things Matter to make the science on toxic chemicals publicly accessible. They produce videos to show how human health is inextricably connected with exposures to toxic chemicals and to elevate efforts to prevent disease.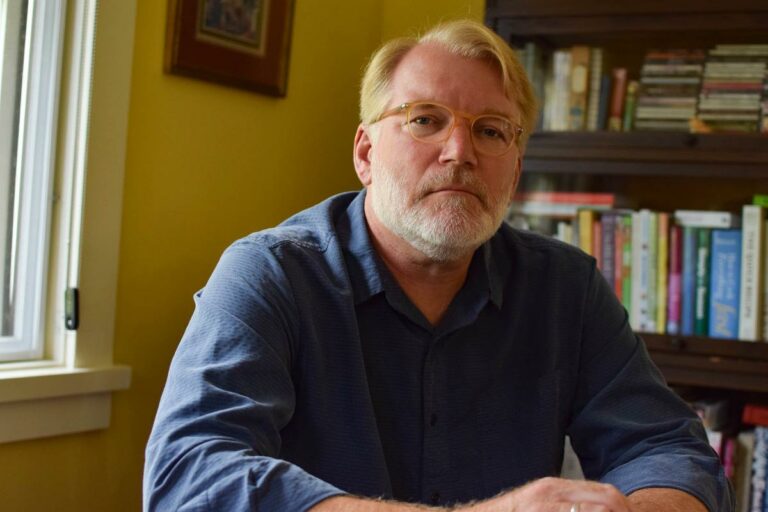
Bruce Lanphear, a health sciences professor at Simon Fraser University and an expert on lead toxicity.
Listen to the Podcast:
The podcast of this program will be available Monday, February 17, 2025, after broadcast on Feb. 15. You can stream the show from this site and download the podcast for free.
13 February 2025, 4:16 pm - 59 minutes 42 secondsShow 1417: Examining the Pros and Cons of Water Fluoridation (Part 1)
This week, we offer the first of a two-part series on water fluoridation. The practice of adding fluoride to drinking water to prevent tooth decay has been controversial for some time. Why? What should we know about it?
You could listen through your local public radio station or get the live stream at 7 am EDT on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on February 10, 2025.
Examining the Pros and Cons of Water Fluoridation:
Tooth decay is uncomfortable. When it leads to periodontal disease and tooth loss, it can have a negative impact on cardiovascular and cognitive health, as well as quality of life. Fluoridation has been employed as a public health intervention to improve dental health. What is fluoride and how does it work? Our guest, Dr. Gary Slade, explains the mechanisms that help fluoride strengthen tooth enamel. In particular, it becomes incorporated into the crystalline structure of the enamel in places where it has been attacked by acid.
It is very difficult to determine exactly how effective water fluoridation may be at reducing dental problems because it started before there were randomized controlled trial conducted. Comparing countries that use this technique to those that do not is imperfect, since there are often many other differences among them. One important difference could be the rigor of data collection and analysis. The only way to overcome that problem is to conduct a randomized controlled trial.
Conducting A Randomized Controlled Trial of Water Fluoridation:
Dr. Slade and his colleagues have already begun exactly such a trial in Lenoir County, North Carolina. Families are assigned to either fluoridated or unfluoridated water. Because each household is provided with big 5-gallon jugs of water for their consumption, they have no way of telling which group they belong to. Nor does anyone else. This creates an effective “double-blind” situation for the trial. The investigators don’t yet have data on dental outcomes. That will be forthcoming, and it will provide a much better assessment of exactly how well fluoridation protects teeth.
Other Ways of Preventing Decay:
Joe recalls the dentist of his childhood cautioning him to avoid sugar. Dr. Slade agrees that limiting the number of times a day that one consumes sweet snacks or sugar-sweetened beverages can make a difference in reducing tooth decay. We asked him to explain the difference between “caries” and “cavities.” Caries is the term for the process of tooth surface deterioration. A cavity is the result of that process. Cutting the amount of sugar we eat can definitely discourage that process.
Clearly, brushing teeth is critical to keeping them healthy. We discussed the amount of fluoride toothpaste we need to put on the toothbrush. It’s not nearly as much as depicted in toothpaste commercials. Dr. Slade also explained that flossing is most impactful when it comes to gum health rather than preventing caries. That is important, too. Healthy gums make it easier to keep your teeth and also promote general health.
A Hint of the Cons of Water Fluoridation:
Fluoridated water is the primary source through which we are exposed to fluoride. On the other hand, it is not the only source. Next week’s guest points out that formula-fed infants get a much higher dose, relatively speaking, than adults if their formula is made with tap water. In addition, we are all exposed to fluoride from nonstick pans and stain-resistant fabrics, antidepressants and anesthetics and a host of other sources. Next week, Dr. Bruce Lanphear will explain why he thinks this is a problem.
This Week’s Guests:
Gary D. Slade, BDS, DDPH, PhD, is the John W. Stamm Distinguished Professor of Dentistry at the University of North Carolina Adams School of Dentistry in Chapel Hill, NC. He conducts epidemiological studies of oral diseases including public health interventions for prevention of dental decay. His website is
https://dentistry.unc.edu/people/gary-slade/
Gary Slade, BDS, DDPH, PhD, is the John W. Stamm Distinguished Professor of Dentistry at the University of North Carolina Adams School of Dentistry in Chapel Hill, NC.
Bruce Lanphear, MD, MPH, is Professor of Health Sciences at Simon Fraser University in Burnaby, BC. His website is https://www.sfu.ca/fhs/about/people/profiles/bruce-lanphear.html
Bruce Lanphear, a health sciences professor at Simon Fraser University and an expert on lead toxicity.
Listen to the Podcast:
The podcast of this program will be available Monday, February 10, 2025, after broadcast on Feb. 8. You can stream the show from this site and download the podcast for free. Next week, the show will focus on Dr. Lanphear’s research.
7 February 2025, 1:07 am - 1 hour 13 minutesShow 1416: Exposing Fraud and Arrogance in Alzheimer’s Research
This week, we explore the evidence that some respected researchers in the field of Alzheimer’s disease took shortcut or even manipulated their data to get the results they wanted. How did our guests detect fraud and arrogance in this research?
You could listen through your local public radio station or get the live stream at 7 am EDT on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on February 3, 2025.
Exposing Fraud & Arrogance in Alzheimer’s Research:
With nearly seven million Americans currently suffering from Alzheimer’s disease, the effort to understand what causes it and how it could be treated effectively is urgent. Over the last several decades, research on this dementia has focused largely on amyloid plaque (also called amyloid-beta) in the brain as the sole cause. Consequently, drug companies have developed medications that can pull plaque out of the brain. Medicines like aducanumab (Aduhelm), lecanemab (Leqembi) and donanemab (Kisunla) do that pretty well. Unfortunately, though, the patients don’t get better. At best, they decline a little more slowly. Could putting all the focus on amyloid-beta have been a mistake?
Western-Blot Images Appear to Have Been Changed:
Dr. Matthew Schrag is a neurologist who has been examining images in scientific papers independently of his university duties at Vanderbilt. His initial investigations were of studies of a drug called simufilam being developed by Cassava Sciences. He detected signs suggesting that some of the images (termed “Western blot”) indicating proteins present in certain tissues had been altered. To interpret such images appropriately, a person needs a high level of expertise. Changing the picture can change the interpretation of the data as well.
The Risks of Blowing the Whistle:
An investigative journalist for Science magazine, Charles Piller, heard about Dr. Schrag’s discoveries and wrote an in-depth story about it. Dr. Schrag had not set out to be a whistleblower. Both he and Mr. Piller were well aware of the hazards whistleblowers can run, especially if they are early in their careers. However, they are both curious people and dedicated to research integrity. Dr. Schrag had found some disturbing signs in foundational papers of the field. Charles Piller thinks of him as the most important whistleblower in the history of Alzheimer disease research.
The two men teamed up to take a closer look. What could account for the apparent image manipulation that they uncovered? As Mr. Piller observes, the incentives for scientists encourage data manipulation if one is so inclined. Getting journals to retract published papers is difficult. Universities are likewise not eager to investigate prominent investigators. Mr. Piller and Dr. Schrag are careful not to imply that the field is rife with fraud and arrogance. However, they found far more than we should be comfortable with.
Verification:
Mr. Piller invited other experts to review the images that Dr. Schrag had flagged as questionable. In most cases, they agreed that someone had apparently tinkered with them. In some cases, images reappeared in multiple papers. Since they are an important form of data, they should not be replicated in papers describing different experiments.
The Problems with Amyloid Drugs:
It seems very odd that the FDA approved aducanumab (Aduhelm) despite the recommendation of its expert panel not to do so. Aduhelm has since been removed from the market. Like other drugs in the class, it has a small benefit–almost imperceptible from the perspective of the patients or their families. The side effects could be consequential, however. In some cases, the drug causes swelling or bleeding of the brain. It also can result in ARIA, amyloid-related imaging abnormalities. Over time, these medications end up shrinking people’s brains even more than the disease itself does.
The Future of Research on Alzheimer’s Disease:
Once fraud and arrogance have been exposed, suspicious findings could be excised from the scientific literature. This should permit research to flourish on a range of approaches to understanding Alzheimer’s disease.
This Week’s Guests:
Matthew Schrag MD, PhD, is Assistant Professor of Neurology at Vanderbilt University School of Medicine and Director of the Cerebral Amyloid Angiopathy Clinic. The Schrag Lab is focused on discovering shared molecular pathways between Alzheimer disease and cerebral amyloid angiopathy. His website is https://medschool.vanderbilt.edu/brain-institute/person/matthew-schrag-m-d-ph-d/
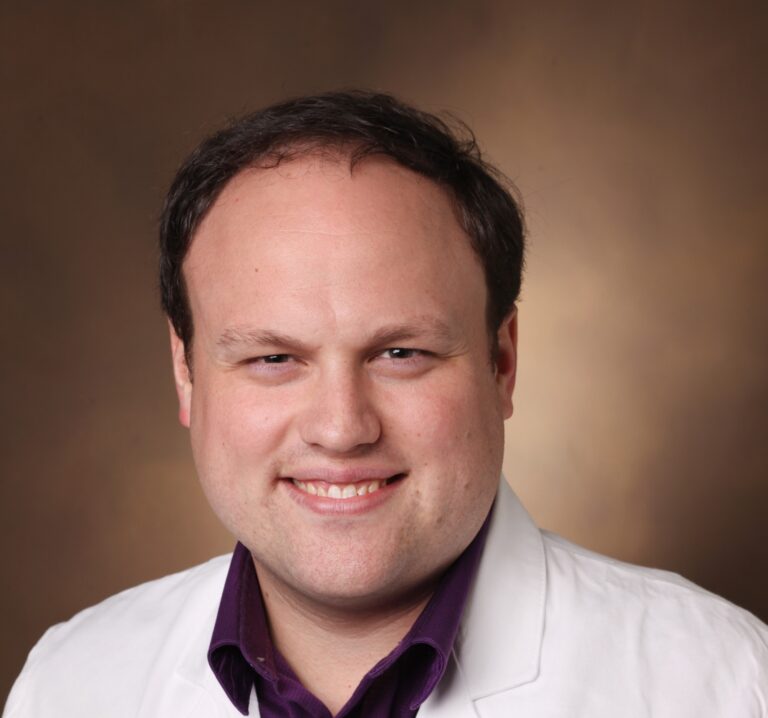
Matthew Schrag, MD, PhD, Vanderbilt University
Charles Piller is a prominent investigative journalist, primarily known for his work in the field of science. He writes in-depth stories for Science magazine, where he often exposes misconduct and problematic practices within scientific research, particularly focusing on public health issues like the study of Alzheimer’s disease. Charles Piller is the author of Gene Wars and The Fail-Safe Society. His most recent book is Doctored: Fraud, Arrogance, and Tragedy in the Quest to Cure Alzheimer’s.
The People’s Pharmacy is reader supported. When you buy through links in this post, we may earn a small affiliate commission (at no cost to you).
You can read an essay by Charles Piller recently published in The New York Times: “The Devastating Legacy of Lies in Alzheimer’s Science.” The photo of Charles Piller is by Mike McGee.

Charles PIller, author of Doctored: Fraud, Arrogance and Tragedy in the Quest to Cure Alzheimer’s
Listen to the Podcast:
The podcast of this program will be available Monday, February 3, 2025, after broadcast on Feb. 1. You can stream the show from this site and download the podcast for free. This week, you’ll hear Charles Piller describe why the operation of FDA’s Center for Drug Evaluation and Research might raise some red flags. We also discuss the monoclonal antibody drugs that the FDA has approved to treat Alzheimer’s disease. In a shift of focus, we examine the incentives that power a nonprofit organization such as the Alzheimer’s Association.
30 January 2025, 8:22 pm - 1 hour 1 minuteShow 1415: Can Home Remedies Help Overcome Cold Symptoms?
This week, Joe & Terry invite listeners to share their favorite home remedies for colds. No one expects a remedy to shorten the duration of a cold–although perhaps one or two could! But many may help people feel better for a few hours if they alleviate symptoms. You can call in your suggestions to 888-472-3366 between 7 and 8 am EST on Saturday, January 25, 2025. Or you can send them by email: radio@peoplespharmacy.com
You could listen through your local public radio station or get the live stream at 7 am EDT on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on January 27, 2025.
Home Remedies for Cold Symptoms:
If you start to come down with a cold, what do you do? A lot of people reach for acetaminophen or ibuprofen, especially if they are running a mild fever. We suggest saving the pain relievers for when you have pain and welcome a fever. It is your body’s way of fighting off infection and shouldn’t need treating unless it gets really high. Does your family have a remedy like piling on the quilts designed to get the cold victim to actually run a fever? Some people turn to hot liquids to warm up when they have a cold.
Chicken Soup and Golden Milk:
Around the world, people rely on chicken soup when they have a cold. Inhaling the steam from a bowl of soup can help ease congestion temporarily. If you make your soup with lots of thyme, it may reduce coughing for a while. In China, grandmothers often make chicken soup with astragalus root, because that has a reputation for bolstering the immune response.
Vegetarians avoid chicken soup, of course, but some embrace golden milk. This traditional Ayurvedic cold remedy includes the yellow spice turmeric mixed into warm milk and sweetened with honey to taste. Just as with chicken soup, people who grew up with this remedy find it a true comfort when they are under the weather. Researchers have found that curcumin, a key component of turmeric, has definite antiviral activity (Molecules, July 8, 2022).
Several Varieties of Tea:
We have some favorite types of tea that we like to use if we feel a cold coming on.
Ginger Tea for Cold Symptoms:
Ginger tea is a lovely way to address both cough and congestion. You can make it from dried ginger, but we think it is best made by grating fresh ginger root and steeping it in hot water. If you like, it can be sweetened with honey. Some people prefer to add a bit of hot pepper, livening an already spicy drink even more.
Thyme Tea for Cough:
When we start to cough, we rely on a cup of fresh-brewed thyme tea. Using a half teaspoon of dried thyme leaves in a tea infusing spoon, we steep 6 ounces of hot water for about five minutes. This is delicious when we add lemon (and honey!). We find it really calms a cough quickly for several hours. There haven’t been many studies of this herbal remedy, but one randomized, triple-blind, placebo-controlled trial in kids with asthma found that thyme syrup reduced activity-induced cough (Allergologia et Immunopathologia, Jan. 2024). These youngsters have asthma, so it is not directly applicable to people with coughs due to colds; still, it suggests there is some activity.
Elderflower Tea:
Extracts of dried flowers of elderberry shrubs (AKA elder flower tea) contain high levels of polyphenols (Journal of Agricultural and Food Chemistry, Feb. 11, 2015). Some scientists are interested in developing medicinal compounds to treat respiratory infections based on the components of elderberries (Molecules, June 22, 2024). Traditional herbalists recommend elder flower tea for a cough associated with a cold. Have you tried this approach?
The Sambucus fruit, elderberry, has been having a moment lately. A systematic review of its use of viral respiratory illnesses found that it doesn’t seem to prevent colds, but it may reduce the duration or severity (BMC Complementary Medicine and Therapies, April 7, 2021). As with nearly all our remedies, more research is needed.
Sage Tea for Sore Throat:
When we talk with Dr. Tieraona Low Dog, she frequently recalls that when she was a child, her grandmother would prepare sage tea when there were colds in the household. Rather than consume it as a hot beverage, the youngsters let it cool and used it as a gargle to ease the pain of a sore throat.
What About Vitamin C?
When it comes to vitamin C, are you pro or con? The benefits of this vitamin against the common cold have been quite controversial for decades. Nobel laureate Linus Pauling was a fan, but many doctors are skeptical, to say the least. The latest review shows that high-dose vitamin C can prevent colds in people doing intense physical activity and decrease the severity of colds by about 15 percent (Polish Archives of Internal Medicine, Jan. 13, 2025). That seems like it might be worth a try, given that vitamin C doesn’t often cause side effects. The authors suggest a self-experiment using 6 to 8 grams a day starting at the earliest hint of cold symptoms. Some people will experience diarrhea at that dose and will need to lower it for their personal protocol.
Will Zinc Help Your Sore Throat?
Back in 1979, a little girl with cancer refused to swallow the zinc tablet she was supposed to take. She sucked on it for hours instead. Surprisingly, the cold symptoms she had been developing disappeared. Subsequent research has confirmed that zinc has antiviral and anti-inflammatory effects (European Journal of Clinical Nutrition, April 2023). Have you tried zinc lozenges to treat your cold symptoms? Tell us how it went.
Do You Take Quercetin for a Cold?
The flavonoid quercetin is available as a dietary supplement. It has a reputation for fighting off viruses, possibly because research has demonstrated that it can inhibit the early stages of viral infection and reduce inflammation (Phytotherapy Research, Jan. 2022). Perhaps this helps explain the popularity of onion syrup as a cold remedy. Many listeners have reminisced about this, which appears to have broad popularity. Have you tried it?
Vicks VapoRub:
No discussion of cold remedies would be complete without mentioning Vicks. It actually was developed (more than a hundred years ago) specifically to help with cough from upper respiratory infections. While the usual approach to using Vicks calls for it to be applied to the chest, a lot of listeners have found that applying it to the soles of the feet is also quite effective for a nighttime cough. Be sure to put on some thick socks so the sheets don’t get greasy from the petrolatum. We suspect the menthol that contributes to its distinctive aroma helps explain why it could work for a cough.
Listen to the Podcast:
The podcast of this program will be available Monday, January 27, 2025, after broadcast on Jan. 25. You can stream the show from this site and download the podcast for free.
24 January 2025, 1:40 am - 1 hour 20 minutesShow 1414: Finding Your Exercise Prescription for LifeThis week, two distinguished exercise physiologists tell us why we each need an exercise prescription for life. Dr. Benjamin Levine has worked with the Dallas Bed Rest and Training Study to discover that three weeks of bed rest hurt fitness more than 30 years of normal life. Dr. Claudio Battaglini provides exercise prescriptions for cancer […]16 January 2025, 4:41 pm
- More Episodes? Get the App